The new "new normal" in pandemic year 3
FDA updates self-test kit instructions, one top expert points to geographic variation in Covid risk, and what about RSV?
Where we’ve been, where we’re headed
Adapting to “normal life” with some precautions
New variants and other risks on the horizon
SARS-CoV-2 began circulating almost three years ago
Within the next few weeks, the world will enter the third year of Covid-19. In the United States and many other places, the majority of people clearly think and act like the pandemic is “over.” The families of the 2,507 Americans who died from Covid in the past week may not agree. But we are far better off than we were just a year ago.
Overall, the combination of widely available and effective vaccines, testing and treatments have rendered this once-frightening disease into a controllable illness. Avoiding a Covid infection is still prudent because of possible illness and long-term symptoms, but we have the tools to avoid severe illness and death, as the White House and CDC keep saying.
Long Covid is worth avoiding. A large study of patients across the Kaiser Permanente health plan population found long-term Covid symptoms in about 1 out of every 4 people who got sick with Covid. The 10 most common long-term symptoms are:
Other lower respiratory disease
Diabetes
Gastrointestinal disease
Conditions associated with dizziness or vertigo
Abdominal pain
Nonspecific chest pain
Mental health
Anxiety disorders
Genitourinary symptoms and ill-defined conditions
Malaise and fatigue
As in other studies, those who had significant underlying medical conditions prior to Covid infection were at the highest risk of significant Covid illness, but some people without any such “co-morbidities” suffer long-term consequences, too. The results were published in Nature Medicine.
For this transformation to occur in less than three years is a tribute to the scientists, physicians, nurses and other health experts responsible for rapidly understanding the novel coronavirus and quickly developing the countermeasures that have allowed most of us to resume many of the activities that were halted in 2020. I consider myself fortunate to work with some of these people in my role as an advisor to one of the U.S. government offices involved in this effort.
Have we figured out where Covid came from?
No, and we likely won’t ever know with absolute certainty, but the most credible explanations point to the virus transmitting to a human at a market that sold wild animals in Wuhan, China. Politicians and others claim that it came from a virology lab. You can expect to hear a lot more about “investigations into the origins of Covid-19” in the months ahead.
This Los Angeles Times column disputes recent findings of a Senate minority report and a Vanity Fair/ProPublica article based on the same research. Those publications said that the virus was likely leaked from a Wuhan lab. However, LA Times columnist Michael Hiltzik says the Senate researcher, who provided documents to Vanity Fair and ProPublica, based much of his conclusion on an incorrect translation of documents in Chinese.
Although there were some reports suggesting that Covid-19 had reached the United States or Europe in 2019, there is not enough reliable data to be sure of this. The first known Covid-19 patient was admitted to a hospital in Wuhan, China on Dec. 1, 2019, and the first alert published outside of China was on December 31, 2019.
Source: Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5. Epub 2020 Jan 24. Erratum in: Lancet. 2020 Jan 30;: PMID: 31986264; PMCID: PMC7159299.
What “new normal” looks like for us: live normally but test frequently, take precautions when local Covid rates rise
Now that most Americans have either had Covid-19 or have been vaccinated, or both, most Americans have some immunity against Covid. However, as we have seen in recent months, the omicron variant has been adept at infecting people — even if they had been vaccinated or had previous Covid-19 infection. Only about 5% of Americans have received the “bivalent” booster, which protects against omicron, which is why Covid keeps getting transmitted. With every transmission, the risk of new variants increases. This means that “herd immunity” just isn’t going to happen anytime soon, especially when 20% of us aren’t getting vaccinated. Such is our life.
At the same time, Covid simply isn’t as scary as it was. If you get Covid, physicians and nurses know how to take care of you. In fact, now widely available Paxlovid has proven to be remarkably effective at reducing severe illness among people who are most at risk. (Its benefit for people under 50 and without underlying medical conditions has not been established.) There are other treatments, too. (And the relatively few people who have “Paxlovid rebound” still fare better than those without the treatment.)
The bottom line is that those of us who are fully vaccinated, including with a booster shot since September 2022, and who do not have serious underlying medical conditions can be reasonably comfortable going out and about, interacting with others, and even attending indoor or outdoor gatherings.
But keep those masks handy, and check local data before going to an indoor gathering. Exposure to one or more infected people for 15 minutes or more remains risky. For me, this means I’ll put on my mask when close to others while traveling or shopping, and I’ll continue to avoid indoor dining when outside the San Francisco area. Here’s UCSF’s Dr. Bob Wachter’s take:


Wachter is correct, the rates of Covid cases and deaths varies widely by region. In the past week, more than 280 people in North Carolina died, 157 in Michigan. The pandemic is not over, not yet. This is even more true in other countries, where vaccinations have been harder to distribute.
How useful are those home tests for Covid?
There’s been a lot of confusion over testing, and many people may be concerned that the home tests are inaccurate. In fact, the home tests authorized by the FDA are helpful - and detect Covid-19 about 80% of the time, when used properly and when the results are understood. Key point: a negative result does not definitively show that you are not infected or contagious.
Use a self-test before going into a gathering that includes vulnerable people, and consider using a test routinely if you interact with a lot of different people. Home antigen tests are widely available — and free, for many people.
Instructions for self-test kits will soon be updated with more specific guidance on repeat testing. The FDA specifies:
If a person has Covid-19 symptoms, at least 2 tests should be done over 3 days with at least 48 hours between tests.
If a person does not have symptoms but suspects possible infection, then they should do three tests over 5 days, with 48 hours between tests.
This FDA article explains more about the home tests for Covid-19 and the risk of false negative results. This link points to a study on how the self tests compare to other testing.
Variants, other viruses on the horizon
With more people out and about, other viruses are getting around with them. As predicted, this year’s flu season is off to a fast start, especially in the southeast and south-central regions. And, an illness known as RSV (respiratory syncytial virus) is sending a lot of kids to hospitals. The CDC published a health alert on Friday, urging healthcare providers to encourage patients to get flu and Covid vaccinations and take other precautions to reduce hospitalizations this winter.
And Covid-19 continues to evolve. Remember when we thought the vaccinations were going to end the pandemic in 2021? Then delta changed everything, and omicron made it worse. Omicron causes almost all cases of Covid now, and it continues to mutate. The World Health Organization is tracking six omicron “sub-variants” to determine if these or other variants differ enough from earlier variants to evade immunity or treatments or cause different disease characteristics.
But wait, there’s more.
Bird, or avian, flu outbreaks have been reported in 43 states in 2022, according to the CDC. Risk to humans is low, but the disease spreads rapidly among birds and can have catastrophic consequences for commercial poultry farmers. “Since early 2022, more than 49 million birds in 46 states have either died as a result of bird flu virus infection or have been culled (killed) due to exposure to infected birds,” says the CDC.
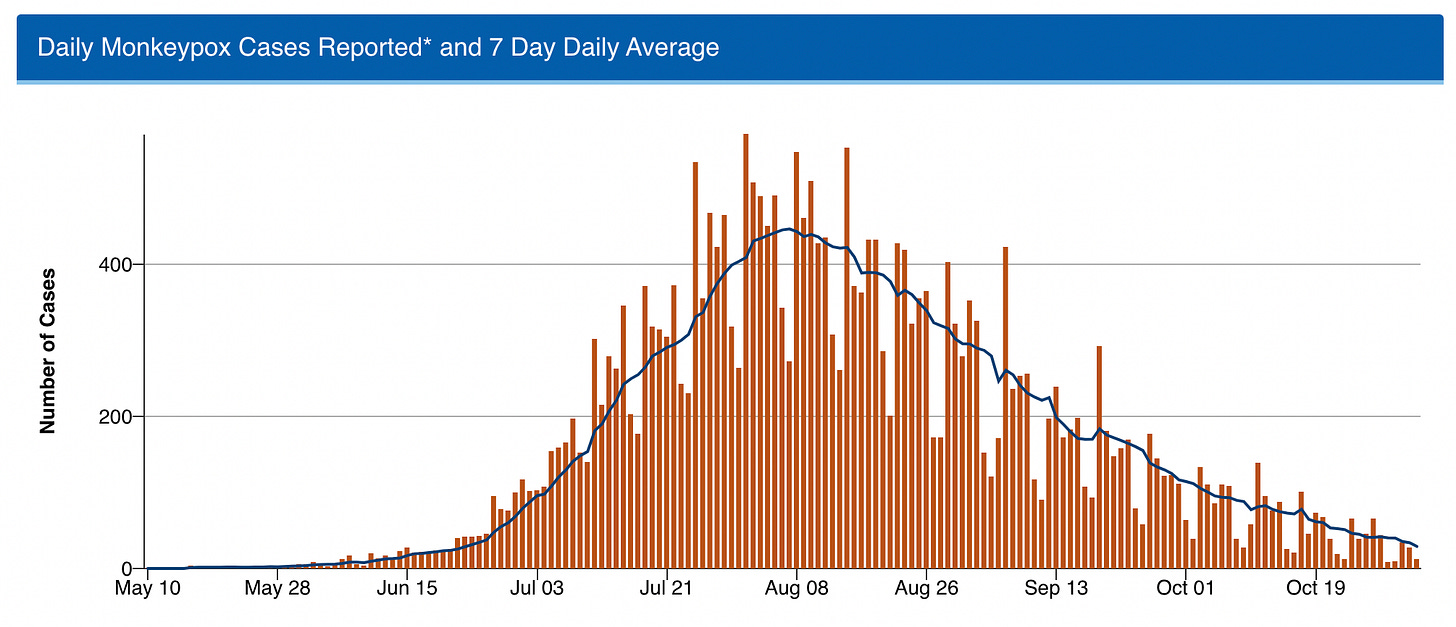
Fortunately, the monkeypox outbreak appears to have been turned around with wider distribution of vaccines, treatments and preventive guidance. Unlike Covid, the U.S. had vaccines and treatments that work against monkeypox on-hand when the first case emerged.
What do you think of this newsletter? Your comments, likes and shares make it possible to continue. Thank you for being part of this community.