Settling-in to our new Covid reality
With restrictions lifted, COVID protection mostly left to individual choices; immunocompromised, elderly most at-risk; And, what about monkeypox?
“The COVID-19 pandemic has now shifted to a new phase, due to the widespread uptake of highly effective COVID-19 vaccines, the availability of effective therapeutics, and the accrual of high rates of vaccine- and infection-induced immunity at the population level in the United States.” - CDC
With the CDC’s decision to lift COVID-19 testing requirements for international travelers effective today, nearly all COVID restrictions have been relaxed across the USA and in many other countries. One way to look at this is that the authorities have accepted the fact that we failed to control COVID-19 and must find ways to co-exist.
In the USA, this may be possible now that safe and effective vaccines and antiviral medicines are widely available. If this is our new reality, what does this mean for you and me? Answers to that and other news below, but first:
Dear Readers:
You may have noticed that it’s been awhile since the last edition of this newsletter. If you are a paying subscriber, don’t worry — you haven’t been billed, and if you are pre-paid, your subscription is automatically extended by the duration of the pause. How useful are these newsletters to you? Should I continue to focus on COVID-19 or would you like me to include other topics? Your feedback will guide the future of this publication. Thank you for your support.
We failed at containment and control, so it’s up to each of us now
I’m writing this while on a flight where very few people are wearing masks. This is despite new cases rising again in the area towards a second peak after the dramatic surge seen in January. Even with higher numbers of new cases and hospitalizations, the San Francisco area still has recorded few COVID-19 deaths compared to other regions. Most importantly, the rate of new cases is more than twice as high among unvaccinated than vaccinated individuals. While this is the same story we’ve been seeing and experiencing for more than a year, there are some important shifts within certain groups and the number of severe cases and deaths remains low — but not zero.
Key points:
The currently circulating variants are more transmissible, which means that your risk of infection may be higher than before. Risk remains higher in communities with fewer people vaccinated.
Because most Americans have some immunity from vaccines or prior infection, most people who get infected have milder disease than would have occurred several months ago. Older and those with underlying health conditions remain at higher risk.
As long as many Americans remain unvaccinated, the virus is likely to continue to evolve and evade protection.
Although there’s plenty of work being done on possible new vaccines, it’s unlikely that there will be a variant-specific or other new Covid vaccine in the near-term.
Health experts warn that although the current wave is at or near its peak, conditions are ripe for another surge in the Fall.
Here’s my best guidance (always check with your own healthcare provider for advice specific to your situation:)
Get vaccinated and boosted. The data is overwhelmingly clear that three doses of the Pfizer or Moderna vaccines save lives. Talk to friends and family about this, as personal conversations are highly effective at overcoming vaccine hesitancy.
FDA advisors meet this week to consider whether to recommend the Pfizer and Moderna vaccines for very young children. If the FDA authorizes these vaccinations, the CDC is expected to issue clinical guidelines in time for vaccinations to begin as soon as June 21.
If you have young children, contact your pediatrician’s office to find out how and when you can get them vaccinated. There also will be pop-up clinics organized by children’s hospitals, museums and other community organizations.
Protect those around you.
If you are sick — sniffles, coughs, anything — please stay away from other people.
Use self-tests (antigen tests) regularly, and especially before going into a group or multigenerational family event.
If you think you might have been exposed to Covid, wear a mask if going out in public.
Consult your healthcare provider promptly if you think you’ve been exposed to COVID-19 or if you test positive. There are treatments available but they only work when taken in the first 1-3 days of illness.
Tests are helpful but not definitive. Probably everyone of us has heard of someone recently who got Covid even though they tested negative, or people who tested negative on a self-test only to test positive 10-12 hours later.
Err on the side of caution if you are or were infected. Isolation sucks, but giving a potentially dangerous disease to others is probably worse.
If you are immunocompromised, you can’t rely on public health guidelines for protection, since vaccine and mask mandates have dropped, and there are plenty of examples of infected individuals going out in public without masks. Unfortunately, this means you probably will want to wear a good mask more than most others.
Check the CDC’s guidance for your local area.
Wear N95 or KN95 masks anytime you think there might be Covid around you.
The latest variants are highly transmissible, so consider masking even outdoors if you are likely to be close to others.
The USA’s transition from pandemic to post-pandemic
If you go back to Spring 2020, public health officials were still trying to contain COVID-19 by identifying new cases, isolating infected individuals and reducing risks of transmission through “non-pharmaceutical interventions” such as social distancing, handwashing, and face coverings. Inconsistent messaging from authorities, unknown characteristics of the novel coronavirus, and interference from politicians were among the factors that caused containment to fail.
Social discord, malfeasance among political leaders and ethically dubious media set the stage for hindering the vaccination campaign, which had the potential to bring the pandemic to its end. Then as the vaccines’ impact started to become clear, the CDC got everyone confused again when it dropped mask recommendations, only to bring them back when the delta and omicron variants emerged.
For more, read what Dr. Eric Topol of Scripps Research Translational Institute published in this insightful article, “Covid Capitulation.”
Because about 1/3rd of Americans haven’t been vaccinated and less than half of those who were vaccinated have gotten boosters, COVID-19 keeps circulating — and as it evolves, gets much better at evading immunity from vaccines or natural infection. The good news is that the vaccines have continued to provide excellent protection against severe illness and death, and for those who do get sick, Paxlovid and other new treatments are helping people recover. But the continued refusal of vaccinations means hundreds of people are dying every day — and most of those deaths could have been prevented.
Although the data and the consequences may be similar, the reasons for vaccine refusal have shifted, according to the vaccine tracking surveys by the Kaiser Family Foundation.
71% of unvaccinated adults consider themselves “very safe” when working outside their homes, compared with 48% of vaccinated adults.
The percentage of Republicans who “definitely will not get” COVID-19 vaccinations has risen from about 23% a year ago to 37% in April.
More than 60% of unvaccinated American adults are white, 47% have high school or lesser education, and 33% identify as evangelicals.
Vaccine hesitancy in minority populations has largely waned.
Misinformation appears to be impacting many vaccination decisions, especially among pregnant people.
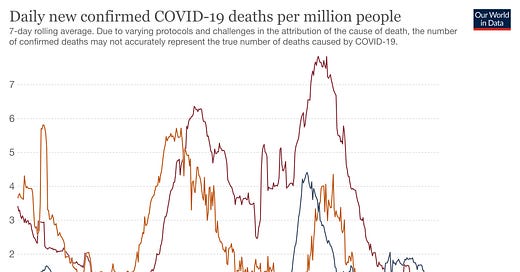
This chart shows deaths per capita in the USA compared with Canada and Mexico since March 2021, when vaccines became widely available in the USA. Deaths rose during the delta and omicron surges, but the rate in the USA has been higher than our North American neighbors throughout the pandemic. The explanation is simple and tragic: the US has been unable to get past 70% of the population vaccinated. Canada, which got a later start on its vaccination program, got 80% of its population vaccinated by the end of 2021, and the death chart shows the corresponding drop in deaths there.
You can explore much more at OurWorldInData.org.
Meanwhile, what about monkeypox?
The short answer appears to be: don’t worry much. It spreads when you have very close contact with someone who has the pox lesions.
However, the clusters of monkeypox cases that have been reported since mid-May in at least 17 states and dozens of other countries are different from prior outbreaks. This raises the possibility that this virus has found new ways to spread, though experts say this remains unlikely. Some experts believe that it can be spread via droplets.
Unlike Covid-19, there are already safe and effective vaccines and treatments that work for monkeypox.
(Disclosure: I am a consultant to a contractor that supports BARDA, the Biomedical Advanced Research and Development Authority, part of the U.S. Department of Health and Human Services.)

Communications lessons from the Uvalde horror
Some of you may be aware that I have worked many years with emergency responders to improve communications and public information during major incidents. There are so many aspects of the Uvalde massacre that are heartbreaking, including the communications failures. While there are many details not yet clear, there are at least five lessons for every public information officer already. Read more in this LinkedIn post.
And there will be a lot more on this and other recent learnings for PIOs in the forthcoming second edition of The Communications Golden Hour: The Essential Guide to Public Information When Every Minute Counts.
Your feedback means a lot
Please share your thoughts on this newsletter or any of the topics raised. Thank you!




Here’s a travel blogger’s thoughts about the CDC decision to drop the testing requirement. While I disagree on her point about testing before domestic flights, she raises good questions.
http://carolapucci-tips.blogspot.com/2022/06/testing-requirement-lifted-for.html
And veteran travel business reporter Joe Brancatelli makes the most important observation: just because something isn’t required doesn’t mean it’s not a good idea to do it anyway.